A novel coronavirus (COVID-19) is spreading rapidly across the world and at one point or another, everyone has experienced a quarantine or “lock down” of some sort since March 2020. It sucked, it still sucks, and unfortunately, it will continue to suck until more and more research is done to produce a viable cure. Whether the pandemic ends next month, next year, or fornever – one thing is certain and that is, we must change how we practice infection control.
In one way or another, humans are resistant to change. A change can be for the better or for the worse, but either way, it disrupts our physical and mental flow when we try to process something new. In light of all the recent changes this year, I am sharing my experience working as a clinical audiologist during the COVID-19 pandemic.
sh!t hit the fan in March 2020. I had just returned from a weekend trip to New York City to celebrate a friend’s birthday when the number of infected cases worldwide began to increase exponentially. News about the first detected case in the United States broke out in late January 2020 and it happened to take place in my home state, Washington. So naturally, I developed extra caution with monitoring myself for the classic symptoms: shortness of breath, dry cough, fever, and/or extreme mind and body fatigue. Fingers crossed, I did not develop symptoms after my trip and I have been symptom-free throughout this whole time.
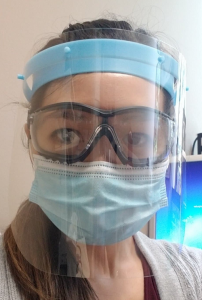
Wearing a mask is ABSOLUTELY necessary
At work, all staff and healthcare providers were heavily encouraged to wear surgical masks even before the World Health Organization declared a pandemic. There was a shortage of N95 masks, but luckily, our manager was able to secure just enough for every member of our clinic to have one. I’m not going to lie – the adjustment to wearing a mask consistently at work was not easy. I remember feeling shortness of breath because I had not gotten used to wearing a mask for prolonged periods of time. And yes, my breath would fog up my glasses and obscure my vision anytime I spoke more than 2-3 sentences. Sure, it may have felt like the mask was suffocating my face for a while, but I got over it quickly because the mask is an effective, protective barrier between myself and my patients.
Our clinic also implemented guidelines that patients had to come in wearing a mask or some kind of face covering. If they didn’t have one, we would provide them with one. If they didn’t want to wear one, we would request that they reschedule their appointment for another time. Patient refusal to wear a mask would compromise the health of our clinic staff and other immunocompromised patients.

Social distancing of 6 feet or more between ALL individuals
Unfortunately, our clinic’s square footage is on the smaller side. We had to figure out a way to space out appointments to avoid having too many patients waiting in the lobby at any one point in time. Some patients opted to wait in the hallway or in their cars until a room was ready for them. Some patients took advantage of provider telehealth services. But many patients canceled or rescheduled their appointments further out into the year to avoid exposure, so clinic activity was unusually quiet for the months of April and May. This wasn’t great for the business, but people were doing what they had to do to exercise caution.
Long gone are the days of handshakes and hugs. Handshakes are ok. I learned how to give firm handshakes over time because that was the professional thing to do. Oh well, it’s not necessary anymore! As for hugs? I personally have never been a fan of giving or receiving hugs from patients. Perhaps I’ve made exceptions for patients that I developed a strong connection with and they always ask before going in for one. Too bad now! I have found the perfect excuse to decline any sort of physical contact with patients, except to touch their ears. I would consider this a win.
Maintaining the appropriate distance from patients can be tough as an audiologist. When doing otoscopy to look into their ear canals, you are literally inches away from the patient’s facial orifices. Ever bend down for a look at the very same moment when said patient decides to cough or sneeze? It has happened in pre-COVID times and I will do whatever it takes to make sure it doesn’t happen now that we are in the middle of a pandemic. Call me silly, but I hold my breath while doing otoscopy or anything that requires me to be less than an arm’s length away from my patients.
Increase use of disinfectant sprays, wipes, and alcohol-based hand sanitizer




Our clinic has been lucky with maintaining a good stock of disinfecting supplies. We wear gloves as much as possible and definitely when we’re using CaviWipes to wipe down surfaces to protect our skin from harsh chemicals and possible pathogens. Hand sanitizer stations are available in every room and every corner of our clinic. That stuff is liquid gold and very effective, but be sure to wash your hands with soap and water too. Nothing feels better than rinsing off that thick, slimy layer of hand sanitizer with warm water and lavender scented antibacterial soap.
We also obtained two UV (ultraviolet) light disinfection boxes, which we use regularly to disinfect our masks for reusability. This was new technology to me and I’ll admit I was pretty skeptical about it at first.

What does UV light do?
It is a special type of electromagnetic radiation that kills all pathogens and germs, including this novel coronavirus, by destroying its genetic makeup. This concentrated energy is dangerous so please, please, please use the equipment with caution because the energy is strong enough to damage human skin.
Effective communication with hard-of-hearing (HOH) patients
People with hearing loss are struggling to communicate now that everyone is required to wear a mask in public spaces. Up until this point, we have always encouraged our patients to utilize visual cues and speech-reading to help them understand what they don’t always hear. Don’t get me wrong – we can still recommend this, but we need to think creatively and modify communication strategies to maximize their speech understanding ability. My counseling has now shifted to focus on these main tips:
- Inform others to speak up and slow down their rate of speech. It’s natural for people to talk fast when they get excited or maybe that’s just how they normally talk. Remind communication partner(s) throughout the conversation as often as necessary.
- Rephrase sentences, rather than repeat. Ask for clarification if it’s hard to keep up with the conversation. Avoid saying “huh?!” and instead, ask the speaker to summarize the main points they are trying to get across.
- Don’t apologize for communication challenges associated with having a hearing loss. Communication is a two-way street and speaking with someone with a hearing impairment should not be considered a ‘burden’. Acknowledge that masks are a communication barrier. Inform people about how they can help you hear better.
- Minimize background noise and other distractions. We live in a noisy world, especially when we’re out in public. Of course, communication in a quiet environment is going to be the most ideal for speech understanding. However, next time you’re at the grocery store and you see your chatty neighbor, know that it’s ok to keep the conversation brief. Suggest continuing your conversation over the phone or through a video call. Remember, social distancing is key! Get the groceries and get out.
- If all else fails, use written communication. It takes more time, but it is the best way to relay important information without miscommunication. In clinic, I will pull up a word document and type out my instructions for those with severe hearing loss. I also “talk with my hands” more to supplement any spoken language. You’d be surprised how easily hand gestures can help facilitate understanding!
Something else I have noticed is that patients with hearing loss think I can’t hear them, so they will pull their mask down to talk to me. It is frustrating. As soon as I catch them on it, I kindly ask them to keep their mask on for my safety and theirs. Very rarely do patients resist my request, but I try my best to convince them and if I can’t, I will quickly wrap up the appointment for my safety. Don’t risk your health anymore than you need to.
Many audiologists have started to wear clear or transparent shield masks for ease of communication. Our clinic has not been able to obtain clear masks, but I hope to be able to get some soon.
Hearing aid retention in the ear and maintenance
Patients who come in for hearing aid clean and checks will usually get a review of how to wear their hearing aids successfully with their mask. Some patients report frustration with wearing glasses, hearing aids, a mask, AND fashionable dangly earrings. This is primarily applicable for behind-the-ear or receiver-in-the-canal hearing aid users. Teach them to develop a system for putting on their gear so that everything doesn’t get tangled up behind their ears. I’ve noticed that new hearing aid users are opting for custom, in-the-ear style hearing aids because they don’t want to risk losing their devices.
Also, stress the importance of regular cleaning of hearing aids and ear molds. The ear is a warm, dark, and moist space where germs love to multiply, so it’s important to practice good hygiene by disinfecting the devices that go in the ear often. AudioWipes are highly recommended for gentle and effective cleaning of devices. There is no guarantee that this will kill all germs or COVID-19 virus, but we also want to be careful and avoid abrasions.
Well, there you have it. This was the quickest rundown of the things I’ve learned to implement and adapt to during this unpredictable pandemic. There’s no signs of infection rates slowing down. There’s a lot more that we need to learn and do to protect ourselves, our patients, and the people we surround ourselves with. Audiologists may not be on the emergency front-lines to provide direct care to infected patients, but we need to stay alert and treat everyone as if they might be able to transmit the virus to us.
Share your tips and tricks with me about working in clinical practice! How are you feeling regarding changes in response to the COVID-19 pandemic?




